Millions of Americans struggle with losing weight for years, which can feel like an uphill battle with no end in sight. Obesity is a disease that affects more than 4 out of every ten adults in the United States.1 The American Medical Association began recognizing obesity as a chronic progressive disease in 2013 and describes obesity as having “multiple pathophysiological aspects requiring a range of interventions.”2 Very true.
Since obesity is a disease, people who suffer from it can benefit from medical intervention. If you are obese and interested in medical management, you should discuss this option with your primary care physician or schedule a consultation with our office. They/we will be able to give you individualized care and recommendations. Of course, we will always recommend some common lifestyle treatment options, including diet and exercise, as the first course of action, but you’ve likely tried these without much success. If these have repeatedly failed, weight loss medication and, ultimately, bariatric surgery may be a good option. Medication and surgery are not for people who need to lose a few pounds. These interventions are only for people who need to lose significant weight.
There are pros and cons to both weight loss medications and weight loss surgery. Your primary care physician may suggest medication as a good option before surgery. Or they may offer you the surgical options if the potential benefit is greater. You will work together to develop a treatment plan that you are comfortable with.
Often people will ask, “Are there any medications that work better than surgery for weight loss?” This question is impossible to answer because what works for one person may not necessarily work for the next. Plus, there is very little research on the effectiveness of weight loss medication versus bariatric surgery. Everyone has different genetic makeup, hormones, metabolism, etc. You and your doctor must consider many factors before starting either option.
Considerations to Take Into Account Before Trying Weight Loss Medication
Healthcare providers use body mass index (BMI) to decide if weight loss medications are appropriate for you. The general guideline to see if someone is a candidate for weight loss medication is that they have a BMI greater than or equal to 30 or a BMI of 27 or greater in combination with weight-related health problems. In most cases, your doctor will want to confirm that you have been working on lifestyle modifications before prescribing medication. It is essential to know that medication is used in addition to diet and exercise. Both weight loss medication and weight loss surgery are not used to replace diet and exercise. The people who are most successful long-term have a dedicated exercise plan regardless of whether they lose weight via medication or surgery.
There are several possible side effects of weight loss medications that should be discussed with your provider and pharmacist before beginning treatment. The most common side effects include nausea, vomiting, diarrhea, constipation, indigestion, abdominal pain, and headache. Your doctor will also consider your medical history and current medications. Weight loss medication may not be appropriate for you if it negatively affects your other medical conditions, interacts with your other medications, or limits your lifestyle.
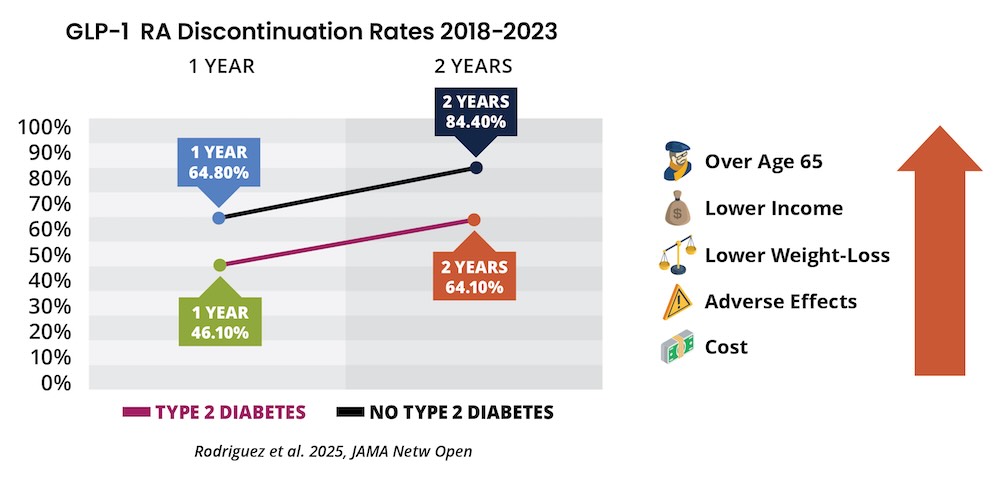
Another consideration, and the possible downfall of weight loss medication, is you will likely gain the weight back after stopping the medication. On the flip side, there have been recent advances in weight loss medication, and the science behind them is getting better.
Medications Approved for Weight Loss
Weight loss medications work by either decreasing appetite, increasing the feeling of fullness, or decreasing fat absorption. Before starting any new medication, you should discuss it with your medical team.
Currently, there are five main medications approved by the United States Food and Drug Administration (FDA) for long-term use for weight loss. These are orlistat (Xenical, Alli), phentermine-topiramate (Qsymia), naltrexone-bupropion (Contrave), liraglutide (Saxenda), and semaglutide (Wegovy). Most recently, tirzepatide, previously approved for type two diabetes, was recently awarded FTA approval for weight loss. Each medication is unique and has its possible side effects.
The Case for Weight Loss Surgery
A successful weight loss operation is a potentially curative procedure, unlike weight loss medications. While only 5 to 10% of dieting patients are successful in the long term, most bariatric surgery patients can keep their weight off long into the future. Of course, the weight loss associated with bariatric surgery can vary. Gastric band and gastric balloon patients may lose up to 30% of their excess body weight (EBW). Gastric sleeve patients may lose up to 60% EBW. A combination of restrictive and malabsorptive procedures like the gastric bypass and duodenal switch has an 80 and 90% excess body weight loss potential.
Of course, surgery comes with potential risks and should not be chosen without significant thought. Most importantly, deciding to have bariatric surgery, while a very personal decision, can be discussed with those around you as you begin the conversation with your medical team and, of course, the surgeon of your choice.
Can Medication Be Used in Postop Life?
The distinct hope is bariatric surgery patients maintain their new and improved lifestyle for years and decades after their surgery. This is the best way to maintain results and improve long-term health. However, some patients may benefit from a boost in their postop weight loss plan with a short course of weight loss medication. This, of course, must be discussed with your primary care physician and bariatric surgeon to ensure safety and effectiveness
The Bottom Line
Results of weight loss medication or weight loss surgery will vary from person to person. Each option has risks and benefits that must be considered along with your medical history and other drugs. It is best to discuss your options with your healthcare provider and develop an individualized treatment plan.
Resources:
- S. Department of Health and Human Services. (n.d.). Prescription medications to treat overweight & obesity. National Institute of Diabetes and Digestive and Kidney Diseases. Retrieved May 20, 2022, from https://www.niddk.nih.gov/health-information/weight-management/prescription-medications-treat-overweight-obesity
- Obesity. AMA. (n.d.). Retrieved May 19, 2022, from https://policysearch.ama-assn.org/policyfinder/detail/obesity?uri=%2FAMADoc%2FHOD.xml-0-3858.xml